Palpitations are heartbeat sensations that feel like your heart is pounding or racing. You may simply have an unpleasant awareness of your own heartbeat, or may feel skipped or stopped beats. The heart’s rhythm may be normal or abnormal. Palpitations can be felt in your chest, throat, or neck.
Normally the heart beats 60 – 100 times per minute. In people who exercise routinely or take medications that slow the heart, the rate may drop below 55 beats per minute.
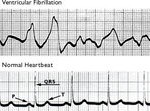
If your heart rate is fast (over 100 beats per minute), this is called tachycardia. A slow heart rate is called bradycardia. An occasional extra heartbeat is known as extrasystole.
Palpitations are usually not serious. However, it depends on whether or not the sensations represent an abnormal heart rhythm (arrhythmia). The following conditions make you more likely to have an abnormal heart rhythm:
- Known heart disease at the time the palpitations begin
- Significant risk factors for heart disease
- An abnormal heart valve
- An electrolyte abnormality in your blood — for example, a low potassium level
Causes
Heart palpitations can be caused by:
- Anemia
- Anxiety, stress, fear
- Caffeine
- Certain medications, including those used to treat thyroid disease, asthma, high blood pressure, or heart problems
- Cocaine
- Diet pills
- Exercise
- Fever
- Hyperventilation
- Low levels of oxygen in your blood
- Heart valve disease, including mitral valve prolapse
- Nicotine
- Overactive thyroid
Home Care
Reducing your caffeine intake will often significantly reduce your heart palpitations. Reducing stress and anxiety can help lessen the frequency or intensity of your heart palpitations. Try breathing exercises or deep relaxation (a step-by-step process of tensing and then relaxing every muscle group in your body) when palpitations occur. Practicing yoga or tai chi on a regular basis can reduce the frequency of your palpitations.
Keep a record of how often you have palpitations, when they happen, how long they last, your heart rate at the time of the palpitations, and what you are feeling at the time. This information may help your doctor figure out both their seriousness and their underlying cause.
Once a serious cause has been ruled out by your doctor, try NOT to pay attention to heart palpitations, unless you notice a sudden increase or a change in them.
If you have never had heart palpitations before, bring them to the attention of your health care provider.
When to Contact a Medical Professional
Call 911 if:
- You lose and regain consciousness.
- Someone with you loses consciousness.
- You have shortness of breath, chest pain, unusual sweating, dizziness, or lightheadedness.
Call your doctor right away if:
- You feel frequent extra heartbeats (more than 6 per minute or coming in groups of 3 or more).
- You have risk factors for heart disease, such as high cholesterol, diabetes, or high blood pressure.
- You have new or different heart palpitations.
- Your pulse is more than 100 beats per minute (without exercise, anxiety, or fever).
What to Expect at Your Office Visit
Your doctor will take a medical history, perform a physical exam, and do an electrocardiogram.
If you have chest pain, shortness of breath, or other worrisome symptoms, and are in the emergency room, your cardiac rhythm will be monitored. An emergency intervention will be performed if necessary to restore normal cardiac rhythm.
If you do not have the symptoms at the time of your visit, the doctor will want to know what your pulse was at the time you felt the palpitations and whether or not the rhythm felt regular.
You may be asked:
- Do you feel skipped or stopped beats?
- Does your heart rate feel slow or fast when you have the palpitations?
- Do you feel a racing, pounding, or fluttering?
- Is there a regular or irregular pattern to the unusual heartbeat sensations?
- Did the palpitations begin or end suddenly?
- When do the palpitations occur? In response to reminders of a traumatic event? When you are lying down and resting? When you change your body position? When you feel emotional?
- Do you have any other symptoms?
As part of your physical exam, your doctor will check your temperature, pulse, breathing rate, and blood pressure. Special attention should be paid to your heart and lungs.
Diagnostic tests that may be performed include:
- Electrocardiogram
- Ambulatory cardiac monitoring (for example, wearing a Holter monitor for 24 hours, or another type of monitor for two weeks or longer)
- Echocardiogram
- Electrophysiology study (EPS)
- Coronary angiography
If your doctor finds you have an abnormal heart rhythm, write down what it is called and be sure to tell other professionals involved in your medical care.
Prevention
 Try to reduce stress and risk factors for heart disease:
Try to reduce stress and risk factors for heart disease:
- Don’t smoke.
- Eat a well-balanced, low-fat diet.
- Exercise regularly.
- Try stress management techniques such as yoga, tai chi, or meditation.
- Make sure that your blood pressure and cholesterol are under control.