Acute leukemia can be divided into two types, depending on the subtype of bone marrow cells affected. If immature cells that produce white blood cells, called lymphocytes, are affected, the leukemia is acute lymphoblastic or lymphocytic leukemia (ALL). This form of leukemia can occur at all ages but is most common in children. With modern treatment programs, a high percentage of children and adults can be cured.
The second type is acute myeloid or myelogenous leukemia. This disease can affect other cells in the bone marrow that are not lymphocytic.
Almost all cases in leukemia in children are acute leukemias, the majority being ALL.
Acute leukemia is not one disease but actually a group of closely related diseases that affect bone marrow cells. These diseases can cause varying symptoms and manifestations. Treatments can be tailored for the characteristics of the leukemia. Different subtypes of acute leukemia have different prognoses.
Acute lymphoblastic leukemia
Acute lymphoblastic leukemia (ALL) is a form of leukemia, or cancer of the white blood cells characterized by excess lymphoblasts.
Malignant, immature white blood cells continuously multiply and are overproduced in the bone marrow. ALL causes damage and death by crowding out normal cells in the bone marrow, and by spreading (infiltrating) to other organs. ALL is most common in childhood with a peak incidence at 2–5 years of age, and another peak in old age. The overall cure rate in children is about 80%, and about 45%-60% of adults have long-term disease-free survival.
Acute refers to the relatively short time course of the disease (being fatal in as little as a few weeks if left untreated) to differentiate it from the very different disease of chronic lymphocytic leukemia which has a potential time course of many years. It is interchangeably referred to as Lymphocytic or Lymphoblastic. This refers to the cells that are involved, which if they were normal would be referred to as lymphocytes but are seen in this disease in a relatively immature (also termed ‘blast’) state.
Diagnosis
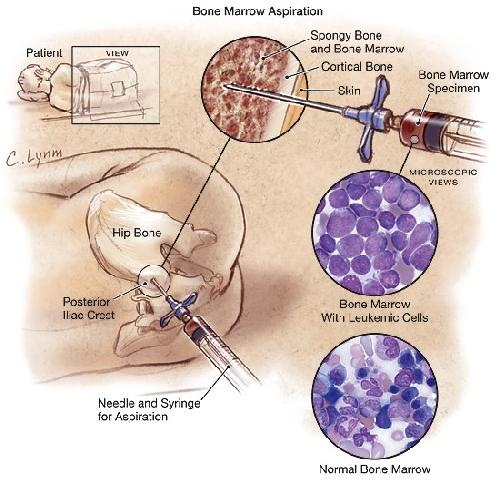
Diagnosing ALL begins with a medical history, physical examination, complete blood count, and blood smears. Because the symptoms are so general, many other diseases with similar symptoms must be excluded. Typically, the higher the white blood cell count, the worse the prognosis. Blast cells are seen on blood smear in majority of cases (blast cells are precursors (stem cells) to all immune cell lines). A bone marrow biopsy is conclusive proof of ALL. A lumbar puncture (also known as a spinal tap) will
tell if the spinal column and brain has been invaded.
Pathological examination, cytogenetics (particularly the presence of Philadelphia chromosome) and immunophenotyping, establish whether the Myeloblastic (neutrophils, eosinophils or basophils) or Lymphoblastic (B lymphocytes or T lymphocytes) cells are the problem. RNA testing can establish how aggressive the disease is; different mutations have been associated with shorter or longer survival. Immunohistochemical testing may reveal TdT or CALLA antigens on the surface of leukemic cells. TdT is a protein expressed early in the development of pre-T and pre-B cells while CALLA is an antigen found in 80% of ALL cases and also in the “blast crisis” of CML.
Medical imaging (such as ultrasound or CT scanning) can find invasion of other organs commonly the lung, liver, spleen, lymph nodes, brain, kidneys and reproductive organs.
Symptoms
Initial symptoms are not specific to ALL, but worsen to the point that medical help is sought. They result from the lack of normal and healthy blood cells because they are crowded out by malignant and immature leukocytes (white blood cells). Therefore, people with ALL experience symptoms from malfunctioning of their erythrocytes (red blood cells), leukocytes, and platelets. Laboratory tests which might show abnormalities include blood count tests, renal function tests, electrolyte tests and liver enzyme tests.
The signs and symptoms of ALL are variable but follow from bone marrow replacement and/or organ infiltration.
- Generalized weakness and fatigue
- Anemia
- Frequent or unexplained fever and infection
- Weight loss and/or loss of appetite
- Excessive and unexplained bruising
- Bone pain, joint pain (caused by the spread of “blast” cells to the surface of the bone or into the joint from the marrow cavity)
- Breathlessness
- Enlarged lymph nodes,liver and/or spleen
- Pitting edema (swelling) in the lower limbs and/or abdomen
- Petechia, which are tiny red spots or lines in the skin due to low platelet levels
Pathophysiology
In general, cancer is caused by damage to DNA that leads to uncontrolled cellular growth and spread throughout the body, either by increasing chemical signals that cause growth, or interrupting chemical signals that control growth. Damage can be caused through the formation of fusion genes, as well as the dysregulation of a proto-oncogene via juxtaposition of it to the promoter of another gene, e.g. the T-cell receptor gene. This damage may be caused by environmental factors such as chemicals, drugs or radiation.
ALL is associated with exposure to radiation and chemicals in animals and humans. The association of radiation and leukemia in humans has been clearly established in studies of victims of the Chernobyl nuclear reactor and atom bombs in Hiroshima and Nagasaki. In animals, exposure to benzene and other chemicals can cause leukemia. Epidemiological studies have associated leukemia with workplace exposure to chemicals, but these studies are not as conclusive. Some evidence suggests that secondary leukemia can develop in individuals who are treated for other cancers with radiation and chemotherapy as a result of that treatment.