Anaplastic thyroid carcinoma is a rare and aggressive form of cancer of the thyroid gland.
Causes, incidence, and risk factors
Anaplastic thyroid cancer grows very rapidly and is an invasive type of thyroid cancer. It occurs most often in people over age 60. The cause is unknown.
Anaplastic cancer accounts for only about 1% of all thyroid cancers.
Symptoms
- Cough
- Coughing up blood
- Difficulty swallowing
- Hoarseness or changing voice
- Loud breathing
- Lower neck mass, often noted to be rapidly enlarging
 Anaplastic tumors have a high miotic rate and lymphovascular invasion. It rapidly invades surrounding tissues (such as the trachea). The presence of regional lymphadenopathy in older patients in whom needle aspiration biopsy reveals characteristic vesicular appearance of the nuclei would support a diagnosis of anaplastic carcinoma.
Anaplastic tumors have a high miotic rate and lymphovascular invasion. It rapidly invades surrounding tissues (such as the trachea). The presence of regional lymphadenopathy in older patients in whom needle aspiration biopsy reveals characteristic vesicular appearance of the nuclei would support a diagnosis of anaplastic carcinoma.
Signs and tests
A physical examination almost always show a neck mass.
- A CT scan or MRI of the neck may show a tumor growing from the thyroid gland.
- A thyroid biopsy shows anaplastic cancer.
- An examination of the airway with a fiberoptic scope (laryngoscopy)Â may show a paralyzed vocal cord.
- A thyroid scan shows this mass to be “cold,” meaning it does not absorb a radioactive isotope.
Thyroid function blood tests are usually normal.
Treatment
This type of cancer cannot be cured by surgery. For most patients, complete removal of the thyroid gland does not prolong their life.
Of other treatment options, only radiation therapy combined with chemotherapy give significant benefit.
However, with today’s technology, new drugs, such as combretastatin (fosbretabulin), bortezomib and TNF-Related Apoptosis Induced Ligand (TRAIL), are being introduced and trialed in clinical labs and human clinical studies. Based on encouraging Phase I and II clinical trial results, with combretastatin (fosbretabulin), a type of drug that selectively destroys tumor blood vessels, a large, multi-national clinical trial is being undertaken to determine whether the drug can extend the survival of patients with ATC. Recent studies in Italy have shown positive results against ATC, but more tests outside the lab are needed to confirm this before it can be used in chemotherapy. There have been some case studies where patients with aggressive thyroid cancer have survived outside the mean expected survival time.
Post-operative radiotherapy
The role of external beam radiotherapy (EBRT) in thyroid cancer remains controversial and there is no level I evidence to recommend its use in the setting of differentiated thyroid cancers such as papillary and follicular carcinomas. Anaplastic thyroid carcinomas, however, are histologically distinct from differentiated thyroid cancers and due to the highly aggressive nature of ATC aggressive postoperative radiation and chemotherapy are typically recommended.
The National Comprehensive Cancer Network Clinical Practice Guidelines currently recommend that postoperative radiation and chemotherapy be strongly considered. No published randomised controlled trials have examined the addition of EBRT to standard treatment, namely surgery. Radioactive iodine is typically ineffective in the management of ATC as it is not an iodine-avid cancer.
Imbalances in age, sex, completeness of surgical excision, histological type and stage, between patients receiving and not receiving EBRT, confound retrospective studies. Variability also exists between treatment and non-treatment groups in the use of radio-iodine and post-treatment thyroid stimulating hormone (TSH) suppression and treatment techniques between and within retrospective studies.
Some recent studies have indicated that EBRT may be promising, though the number of patients studies has been small.
Clinical trials for investigational treatments are often considered by healthcare professionals and patients as first-line treatment.
Adjuvant therapy
In the absence of extracervical or unresectable disease, surgical excision should be followed by adjuvant radiotherapy. In the 18–24% of patients whose tumour seems both confined to the neck and grossly resectable, complete surgical resection followed by adjuvant radiotherapy and chemotherapy could yield a 75–80% survival at 2 years.
There are a number of clinical trials for anaplastic thyroid carcinoma underway or being planned.
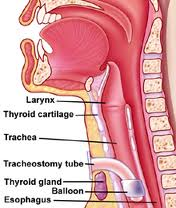
 Surgery to place a tube in the throat to help with breathing (tracheostomy) or in the stomach to help with eating (gastrostomy) may be needed.
Surgery to place a tube in the throat to help with breathing (tracheostomy) or in the stomach to help with eating (gastrostomy) may be needed.
For some patients, enrolling in a clinical trial of new thyroid cancer treatments may be an option.
Support Groups
The stress of illness can often be eased by joining a support group of people sharing common experiences and problems.
Expectations (prognosis)
The prognosis of this disease is poor. Most people do not survive longer than 6 months due to the aggressive nature of this disease and lack of effective treatment options.
The overall 5-year survival rate of anaplastic thyroid cancer has been given as 7% or 14%, although the latter has been criticized as being overestimated.
Treatment of anaplastic-type carcinoma is generally palliative in its intent for a disease that is rarely cured and almost always fatal, with worse prognosis associated with large tumours, distant metastases, acute obstructive symptoms, and leukocytosis. Death is attributable to upper airway obstruction and suffocation in half of patients, and to a combination of complications of local and distant disease, or therapy, or both in the remainder.
Anaplastic thyroid cancer is extremely aggressive; in most cases death occurs in less than 1 year as a result of aggressive local growth and compromise of vital structures in the neck. ATC in most series has a median survival of 4 to 5 months from the time of diagnosis, with rare long-term survivors
Complications
- Spread of tumor within the neck
- Metastasis (spread) of cancer to other body tissues or organs
Calling your health care provider
Call your health care provider if there is a persistent lump or mass in the neck, hoarseness, changing voice, cough, or coughing up blood.