Insulin shock refers to the body’s reaction to too little sugar — hypoglycemia — often caused by too much insulin. Diabetic coma refers to a victim of high blood sugar — hyperglycemia — who becomes confused or unconscious.
These terms are confusing, and not because my blood sugar is too high. They don’t have any connection to reality. Indeed, if I was nicknaming medical conditions today, I would switch these.
Insulin Shock
 Insulin shock makes it sound like the body is in shock, which isn’t true. Shock is, first and foremost, a lack of blood flow to important areas of the body, like the brain. It usually comes with a very low blood pressure. The most common symptom of low blood sugar is confusion (yeah, I know, that’s supposed to go with diabetic coma — just stay with me here), not a low blood pressure. In fact, insulin shock doesn’t affect the blood pressure much at all.
Insulin shock makes it sound like the body is in shock, which isn’t true. Shock is, first and foremost, a lack of blood flow to important areas of the body, like the brain. It usually comes with a very low blood pressure. The most common symptom of low blood sugar is confusion (yeah, I know, that’s supposed to go with diabetic coma — just stay with me here), not a low blood pressure. In fact, insulin shock doesn’t affect the blood pressure much at all.
Insulin shock also implies that insulin is to blame, but insulin — at least from injections — is not required for someone to develop low blood sugar. Plenty of diabetics take pills, which are not insulin, to control their blood sugar levels. Some diabetics control their blood sugar levels simply by watching their diets. To make it even worse, some folks get low blood sugar even though they’re not diabetic at all, which means they would have no reason to take insulin.
The pancreas secrete a hormone called insulin, that maintains the levels of glucose or sugar in the blood. Insulin then stimulates the cells to supply glucose in the blood to various organs in the body. In hypoglycemia or insulin shock too much insulin is secreted by the pancreas, and this leads to lowered blood sugar level (a blood sugar level below 70mg/dL is considered low). Hypoglycemia can also occur if you are taking excess diabetes medications or are eating food that is low on carbohydrates.
 So why is it called insulin shock? Because it sort of looks like shock. Shock, the real, low blood pressure kind, causes the body to react with what’s known as the Fight or Flight Syndrome. Low blood sugar does the same thing. The Fight or Flight Syndrome is the body’s normal reaction to any stress. It makes us ready to run away or fight for our lives. It causes our hearts to beat faster and it makes us sweat.
So why is it called insulin shock? Because it sort of looks like shock. Shock, the real, low blood pressure kind, causes the body to react with what’s known as the Fight or Flight Syndrome. Low blood sugar does the same thing. The Fight or Flight Syndrome is the body’s normal reaction to any stress. It makes us ready to run away or fight for our lives. It causes our hearts to beat faster and it makes us sweat.
Having too little blood, too little oxygen, or too little sugar all make your body scared enough to get ready to do battle or run away. That’s where the name comes from, but it sure doesn’t explain much about the problem.
Severe hypoglycemia or an insulin shock is a medical emergency, and should be treated immediately as it can cause permanent damage to the nervous system. Treating the person with glucose injections is one of the ways to treat insulin shock.
SIGNS & SYMPTOMS: Fast breathing, fast pulse, dizziness, weakness, change in the level of consciousness, vision difficulties, sweating, headache, numb hands or feet, and hunger.
Diabetic Coma
At least with insulin shock, the victim usually knows about the diabetes. Diabetic coma, on the other hand, creeps up on you. It takes a lot of sugar in the bloodstream to reach confusion and unconsciousness. That doesn’t happen overnight. Diabetic coma is most likely to happen to those who don’t know they’re diabetic yet.
Worse, high blood sugar stimulates the production of urine — lots of urine. One of the symptoms of high blood sugar is frequent urination. Victims can urinate so often they become dehydrated, which can lead to shock.
 Okay, so follow along with me here: Insulin shock causes confusion and unconsciousness very quickly and is not shock at all, but diabetic coma only causes unconsciousness after several days — maybe weeks — and leads to dehydration severe enough in some people to be considered shock.
Okay, so follow along with me here: Insulin shock causes confusion and unconsciousness very quickly and is not shock at all, but diabetic coma only causes unconsciousness after several days — maybe weeks — and leads to dehydration severe enough in some people to be considered shock.
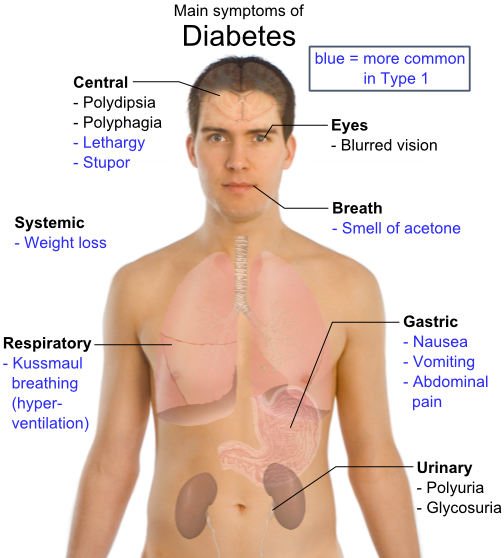
Diabetic coma is a medical emergency, and can prove fatal in case it is left untreated. An extreme fluctuation in the blood sugar level (either too high or too low) is the chief reason for a diabetic coma. Other causes for a diabetic coma are Diabetic ketoacidosis (that is muscle cells do not get enough energy), and Diabetic hyperosmolar syndrome (that is the blood sugar levels cross as high as 600 mg/dL). People with diabetes (type 1 or type 2) are at a risk of diabetes coma. High consumption of alcohol, skipping insulin injections, certain injuries and trauma, and drug abuse are also the risk factors that can lead to a diabetic coma.
SIGNS AND SYMPTOMS: Diabetic coma develops more slowly than Insulin shock, sometimes over a period of days. Signs and symptoms include drowsiness, confusion, deep and fast breathing, thirst, dehydration, fever, a change in the level of consciousness and a peculiar sweet or fruity-smelling breath.