The kidney works to maintain fluid, electrolyte and acid-base balance by eliminating nitrogenous and other metabolic waste products from the body through the urinary system. Another key function of the kidney is to help maintain blood pressure, produce erythropoietin and activate vitamin D. The proper functioning of the kidney is impaired when there is loss of nephrons. The nephron is the functional unit of the kidney. When normal kidney function is greatly impaired, then dialysis becomes necessary.
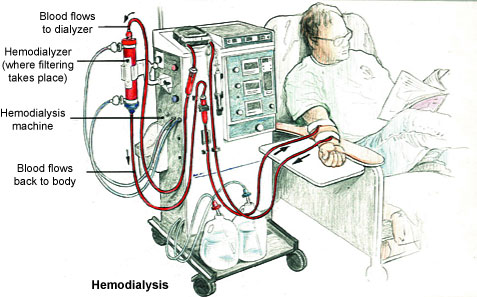
 Dialysis is a process by which waste products are removed from the blood in the event of kidney failure. There are two main forms of dialysis – haemodialysis and peritoneal dialysis. In haemodialysis, blood is cleaned outside the body via a machine. Peritoneal dialysis allows the blood to be filtered through the peritoneal membrane located in the abdomen. The common feature of both types of dialysis is the removal of wastes and excess fluids from the body.
Dialysis is a process by which waste products are removed from the blood in the event of kidney failure. There are two main forms of dialysis – haemodialysis and peritoneal dialysis. In haemodialysis, blood is cleaned outside the body via a machine. Peritoneal dialysis allows the blood to be filtered through the peritoneal membrane located in the abdomen. The common feature of both types of dialysis is the removal of wastes and excess fluids from the body.
In dialysis patients, the ability of the kidney to get rid of waste products and body fluids is compromised. Consequently, a healthy balanced diet is extremely important. The well-being of a dialysis patient depends on taking prescribed medications and on the choice of diet. The right amounts of energy, protein, fluids, vitamins and minerals need to be taken.
Nutritional management
In view of the limited ability of dialysis patients to cope with excess fluid and other metabolic wastes, it is vital that nutrient content of foods consumed by such patients is given special considerations. Nutrient intakes of patients receiving maintenance dialysis are often inadequate, and several lines of evidence suggest that toxins that accumulate with renal failure suppress appetite and contribute to nutritional decline. The nutrients of much relevance for dialysis patients are discussed below.
Protein-energy malnutrition
Malnutrition is common in dialysis patients and close to 40% of dialysis patients suffer from varying degrees of protein-energy malnutrition. Many dialysis patients are not able to meet the minimum energy requirement due to many causes including loss of appetite (anorexia). Decrease in dietary protein and energy intake is one of the main causes of protein-energy malnutrition. The recommended daily protein intake is at least 1.2 g/kg body weight and the optimal energy intake is 35 kcal/kg body weights in patients <60 years, and 30 kcal/kg body weight in patients >60 years. Inadequate dietary prescription, as a direct consequence of some doctors’ preference in prescribing diet restriction rather than providing appropriate nutritional counseling, can actually aggravates malnutrition in dialysis patients. Whereas higher intake of protein requires higher doses of dialysis, lower intake of protein with sufficient energy intake requires lower doses of dialysis, and both could give the same effects on nutritional status. Apart from protein-energy malnutrition, dialysis patients are also vulnerable to micronutrients deficiencies. The process of dialysis itself can cause loss of nutrients especially water soluble vitamins.
Sodium
Diet high in sodium must be avoided because it can make one thirsty and thereby cause the body to hold on onto more fluid. In order to cut down on salt intake one may have to flavour his/her food with herbs and spices instead of common salt. The consequence of high sodium may lead to:
- Swelling of the lower joints of the feet and hands;
- Increased weight associated with accumulated body fluids;
- Increase in blood pressure;
- Shortness of breath and
- Increased activity of the heart.
Phosphorus
Foods rich in phosphorus e.g. dairy products, nuts, beans, lentils, cola drinks, beer, and cocoa drinks are most likely to increase the phosphorus level in the blood. Unfortunately however, dialysis is unlikely to remove accumulated levels of phosphorus in the blood and this can cause the release of calcium from the bones. The continuous removal of calcium from the bones may eventually make them weak causing brittle bones. It is also known that high accumulation of phosphorus in the blood results in the formation of what is called calcium-phosphorus crystals in the joints, muscle, blood, heart etc. The calcium-phosphorus crystals may pose problems such as bone pain, poor blood circulation and even damage to the heart.
Potassium
Equally, persons undertaking haemodialysis may have to limit the intake of foods rich in potassium. Foods high in potassium include bananas, melons, oranges, potatoes, tomatoes, milk, poultry, pork and fish.
Fluids
Factors that can lead to increased intake of fluids must be watched and avoided. Fluids include any food or beverage that remains liquid at room temperature, for example gravy, soups, ice cream, tea, coffee, juices, water, fizzy drinks.
Nutrient supplementation
 Kidney patients on dialysis may have to supplement their diet with vitamins and minerals in order to improve their nutritional status. For example, excess intake of water soluble B vitamins can easily be cleared from the body through the urinary system. Additionally, potassium-restricted or protein-restricted diets may be recommended for some dialysis patients but such diets may result in thiamine (Vitamin B1) and riboflavin (Vitamin B2) deficiencies. Therefore supplementing dialysis patients is a safe way of ensuring deficiency of this group of vitamins is avoided. For thiamine, a supplemental dose of (1.0-1.5 mg/day is adequate. The diet of dialysis patients may be supplemented with vitamin B2 at a dose level of 1.0-2.0 mg/day.
Kidney patients on dialysis may have to supplement their diet with vitamins and minerals in order to improve their nutritional status. For example, excess intake of water soluble B vitamins can easily be cleared from the body through the urinary system. Additionally, potassium-restricted or protein-restricted diets may be recommended for some dialysis patients but such diets may result in thiamine (Vitamin B1) and riboflavin (Vitamin B2) deficiencies. Therefore supplementing dialysis patients is a safe way of ensuring deficiency of this group of vitamins is avoided. For thiamine, a supplemental dose of (1.0-1.5 mg/day is adequate. The diet of dialysis patients may be supplemented with vitamin B2 at a dose level of 1.0-2.0 mg/day.
However, some supplements especially fat soluble ones may be harmful as these can accumulate in the body. Another problem with nutritional supplements for dialysis patients has to do with low compliance. A study carried out in New Zealand showed that patient compliance with nutritional supplements was low and the main barrier was lack of appetite.
Important dietary tips for dialysis patients
- Consume fresh or plain frozen vegetables which often contain no added salt.
- Choose canned fruits which usually contain less potassium than fresh fruits.
- Use non-dairy creamers that contain low phosphorus instead of milk.
- Read labels on food packages to guide in choosing foods with only permissible ingredients.
- Help reduce the salt content of your diet by using herbs and spices instead of common table salt.