Acute pancreatitis refers to the inflammation of the pancreas. The pancreas is not a very “popular†organ, so to speak, since it is not as vital as compared to the other organs such as the heart, the liver, the lungs and the kidneys. Nevertheless, the pancreas which lies behind the stomach does carry important responsibilities in the digestive systems. Certain factors which contribute to acute pancreatitis thus cause one to feel pretty miserable. Let’s have a deeper understanding about this disease.
 What actually does the pancreas do?
What actually does the pancreas do?
The pancreas is a gland which produces enzymes and substances that helps to digest the food we eat. The many different types of dietary intake we consume daily are broken down into substances such as carbohydrate, fats and proteins. The pancreas secretes the necessary enzymes to aid this procedure so that these nutrients can be further be digested and absorbed into our body.
What causes the pancreas to be inflamed?
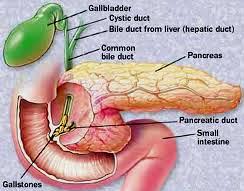
The enzymes in the pancreas are inactive until they are being secreted into the small intestines, where they will then undergo chemical response and become activated to digest the food consumed. Pancreatitis occurs when these enzymes become activated within the pancreas itself, resulting in irritation of the pancreas and hence the uncomfortable signs and symptoms which we will talk about it soon. If such acute pancreatitis recur, tendency of developing chronic pancreatitis, i.e. longstanding scarring of the pancreas, is very likely.
Several factors that have been shown to contribute in the development of pancreatitis:
- Alcoholism
- Cigarette smoking
- Gallstones
- Trauma, e.g. injury to the abdomen
- Scorpion venom
- Endoscopic retrograde cholangiopancreatography (ERCP) – treatment for gallstones can sometimes injure the bile or pancreatic duct causing leakage of pancreatic enzymes
- Steroids
- Infection, e.g. mumps and chicken pox
Signs and symptoms of pancreatitis
The most common symptom that one with pancreatitis would present with is abdominal pain, especially at the upper part or central of the abdomen. The pain comes suddenly and increases in severity, and it may radiate to the back. But such pain could be relieved by positioning of sitting forward.
Vomiting is also a prominent symptom. Some may experience nausea or diarrhea.
Fever is most often presence since there is inflammation going on in the pancreas.

What to expect from the doctor?
First of all, the doctor should rehydrate the patient with intravenous fluids as most likely the patient is dehydrated from the fever and vomiting. Painkillers would also be given to control the pain.
Then the doctor would want to run some investigations in order to help confirm the diagnosis of acute pancreatitis, such as:
- Blood test – to evaluate if the pancreatic enzymes are raised, whether liver function is normal, whether the white blood cells are raised, and to look for any electrolyte imbalance
- Abdominal ultrasonography – to detect gallstones should that be the cause of inflammation
- Endoscopic ultrasonography – a procedure with the same principal as normal ultrasound but with a probe inserted through the esophagus into the small intestine to have a close-up look on the biliary tract and the pancreas. This is useful in detecting any stones in the biliary tract.
Other imaging studies such as computed tomography (CT) scan or magnetic resonance imaging (MRI) are usually reserved for severe cases to rule out complication such as pseudocyst or pancreatic tumor.
Treatment

Aside from the management mentioned earlier, i.e. hydration with intravenous fluids and painkillers, once the diagnosis of acute pancreatitis is confirmed the patient will not be allowed to eat for a few days, until the condition has been fully stabilized. Oxygen will be delivered via a face mask to aid in breathing as some patients may experience some difficulty.
When the cause of inflammation to the pancreas is identified, the main objective of treatment is to treat the cause. Â Depending on the cause, the treatment could be as follow:
 Endoscopic Retrograde Cholangiopancreaography (ERCP)– Since the one of the most common causes of pancreatitis is gallstones, it is necessary for the latter to be removed as soon as possible. This will be done using a camera scope. ERCP is also used to repair the obstructed passage of the bile, of which the mechanical obstruction of the bile duct is also one of the factors contributing to pancreatitis.
Endoscopic Retrograde Cholangiopancreaography (ERCP)– Since the one of the most common causes of pancreatitis is gallstones, it is necessary for the latter to be removed as soon as possible. This will be done using a camera scope. ERCP is also used to repair the obstructed passage of the bile, of which the mechanical obstruction of the bile duct is also one of the factors contributing to pancreatitis.- Treatment and counseling for alcoholism – Aside from gallstones, alcohol is the other culprit that is associated with pancreatitis. It is important to address the problem of chronic alcoholism in order to yield good results of recovery and prevent complications of pancreatitis.