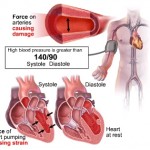
Blood pressure is the amount of force (pressure) that blood exerts on the walls of the blood vessels as it passes through them. Two pressures are measured for a blood pressure reading:
- Systolic blood pressure is a measure of blood pressure while the heart is beating
- Diastolic pressure is a measure of blood pressure while the heart is relaxed, between heartbeats.
How Are Diastolic and Systolic Blood Pressures Measured?
 When measuring these blood pressures, your doctor will likely use a sphygmomanometer. This familiar device with a long name contains a cuff, valve, gauge, and dial. The cuff is wrapped around your arm and then inflated slightly. The systolic and diastolic blood pressures are measured on a gauge attached to the cuff. The measurement blood pressure without further specification usually refers to the systemic arterial pressure measured at a person’s upper arm and is a measure of the pressure in the brachial artery, major artery in the upper arm. Your doctor reads the numbers that appear on the gauge as air is released from the cuff.
When measuring these blood pressures, your doctor will likely use a sphygmomanometer. This familiar device with a long name contains a cuff, valve, gauge, and dial. The cuff is wrapped around your arm and then inflated slightly. The systolic and diastolic blood pressures are measured on a gauge attached to the cuff. The measurement blood pressure without further specification usually refers to the systemic arterial pressure measured at a person’s upper arm and is a measure of the pressure in the brachial artery, major artery in the upper arm. Your doctor reads the numbers that appear on the gauge as air is released from the cuff.
A person’s blood pressure is usually expressed in terms of the systolic pressure over diastolic pressure and is measured in millimetres of mercury (mmHg). The two numbers that measure your blood pressure are written like a fraction: one number on top and one on the bottom. For example, what many people consider normal blood pressure is read as 120/80.
Why Are These Numbers Important?
As blood is pumped from your heart into your blood vessels, enough systolic blood pressure is created to send it to all other parts of your body.
As blood vessels travel away from the heart, they branch off and gradually get smaller — just like a tree’s branches. One branch may go to the brain while another may go to your kidneys.
Systolic blood pressure keeps blood flowing through the branches so that your body’s cells get the oxygen and nutrients they need and waste matter can be removed.
Physiology
 There are many physical factors that influence arterial pressure. Each of these may in turn be influenced by physiological factors, such as diet, exercise, disease, drugs or alcohol, stress, obesity, and so-forth.
There are many physical factors that influence arterial pressure. Each of these may in turn be influenced by physiological factors, such as diet, exercise, disease, drugs or alcohol, stress, obesity, and so-forth.
Some physical factors are:
- Rate of pumping. In the circulatory system, this rate is called heart rate, the rate at which blood (the fluid) is pumped by the heart. The volume of blood flow from the heart is called the cardiac output which is the heart rate (the rate of contraction) multiplied by the stroke volume (the amount of blood pumped out from the heart with each contraction). The higher the heart rate, the higher the mean arterial pressure, assuming no reduction in stroke volume or central venous return.
- Volume of fluid or blood volume, the amount of blood that is present in the body. The more blood present in the body, the higher the rate of blood return to the heart and the resulting cardiac output. There is some relationship between dietary salt intake and increased blood volume, potentially resulting in  higher arterial pressure, though this varies with the individual and is highly dependent on autonomic nervous system response and the renin-angiotensin system.
- Resistance. In the circulatory system, this is the resistance of the blood vessels. The higher the resistance, the higher the arterial pressure upstream from the resistance to blood flow. Resistance is related to vessel radius (the larger the radius, the lower the resistance), vessel length (the longer the vessel, the higher the resistance), blood viscosity, as well as the smoothness of the blood vessel walls. Smoothness is reduced by the build up of fatty deposits on the arterial walls. Substances called vasoconstrictors can reduce the size of blood vessels, thereby increasing blood pressure. Vasodilators (such as nitroglycerin) increase the size of blood vessels, thereby decreasing arterial pressure. Resistance, and its relation to volumetric flow rate (Q) and pressure difference between the two ends of a vessel are described by Poiseuille’s Law.
- Viscosity, or thickness of the fluid. If the blood gets thicker, the result is an increase in arterial pressure. Certain medical conditions can change the viscosity of the blood. For instance, anemia (low red blood cell concentration), reduces viscosity, whereas increased red blood cell concentration increases viscosity. It had been thought that aspirin and related “blood thinner” drugs decreased the viscosity of blood, but instead studies found that they act by reducing the tendency of the blood to clot.
In practice, each individual’s autonomic nervous system responds to and regulates all these interacting factors so that, although the above issues are important, the actual arterial pressure response of a given individual varies widely because of both split-second and slow-moving responses of the nervous system and end organs. These responses are very effective in changing the variables and resulting blood pressure from moment to moment.
Moreover, blood pressure is the result of cardiac output increased by peripheral resistance: blood pressure = cardiac output X peripheral resistance. As a result, an abnormal change in blood pressure is often an indication of a problem affecting the heart’s output, the blood vessels’ resistance, or both. Thus, knowing the patient’s blood pressure is critical to assess any pathology related to output and resistance.